Anti-Smoking Products You Should Know About
Why Products Matter: The Science and Strategy Behind Quitting
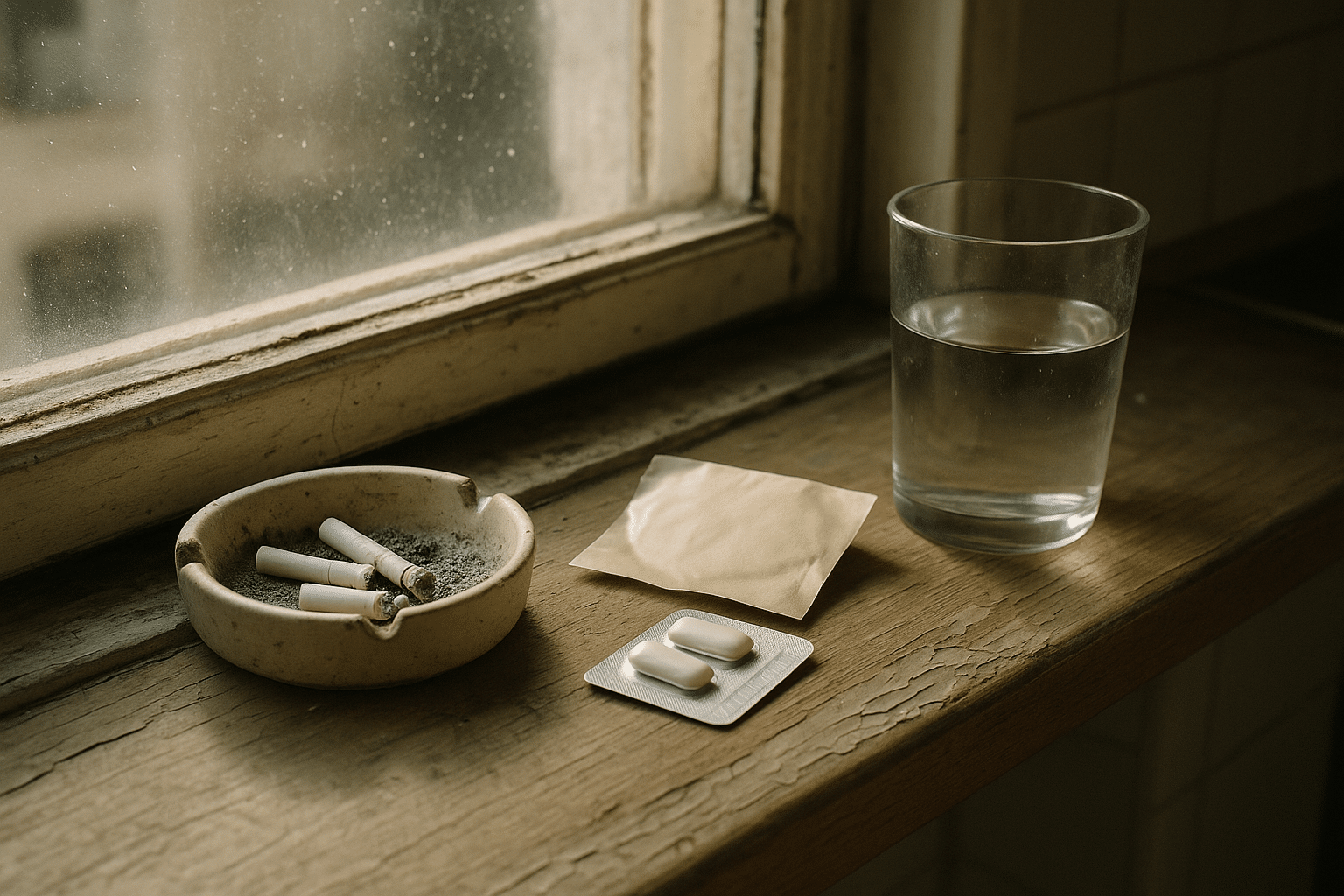
Quitting smoking is one of the most meaningful health moves you can make, yet it rarely happens by willpower alone. Nicotine rewires reward pathways, turning tobacco into a fast, reliable hit that calms stress and sharpens focus—for a moment. Then dependence snaps back with cravings, irritability, and brain fog. That tug-of-war explains why structured tools, from medications to coaching, improve success rates. Within 20 minutes of your last cigarette, your heart rate starts to normalize; within a year, the risk of coronary heart disease drops by roughly half compared with continued smoking. The earlier you quit, the more you gain, but benefits appear at any age.
Think of anti-smoking products as scaffolding that holds you steady while new habits set. Some products ease withdrawal by replacing nicotine in lower, controlled doses. Others dial down the brain’s response to nicotine itself, making cigarettes less rewarding. Behavioral tools teach practical skills: spotting triggers, planning responses, and staying on track after slips. The strongest results often come from a mix—medication plus counseling—because you’re tackling both the biology and the behavior.
Cost and access matter. Many health systems and insurers subsidize quit aids, and pharmacies carry multiple over-the-counter options. Safety matters, too. Most people can use nicotine replacement therapy (NRT) or certain prescriptions, but a conversation with a clinician is wise if you are pregnant, under 18, have heart rhythm problems, uncontrolled high blood pressure, seizure history, or severe mood symptoms. Expect side effects to be mild and front-loaded; they often fade as your body adapts. Quitting is a process with plateaus and small wins worth celebrating.
Here’s the roadmap this guide will follow, so you can jump to what you need:
– Nicotine Replacement Therapy: patches, gum, lozenges, inhalers, nasal sprays—how they work and how to use them together.
– Prescription Medications: varenicline and bupropion—who they suit and what the evidence shows.
– Behavioral Supports and Digital Tools: coaching, quitlines, apps, and trackers—turning motivation into daily action.
– Harm Reduction and Emerging Options: where e-cigarettes, nicotine pouches, cytisine, and alternative methods fit—and where they don’t.
– Choosing Your Path: a practical, stepwise method to pick products and build a plan you can live with.
Nicotine Replacement Therapy (Patches, Gum, Lozenges, Inhalers, Sprays)
NRT supplies nicotine without tar, carbon monoxide, and the thousands of other toxic combustion products in smoke. The idea is simple: keep nicotine levels steady enough to reduce cravings and withdrawal while you unlearn the behaviors that tether cigarettes to coffee breaks, commutes, and stress. A large body of randomized trials shows that using NRT increases the likelihood of quitting compared with going solo, and combining a steady “background” product (like a patch) with a “rescue” product (like gum or lozenges) is often more effective than either alone.
– Patches: Deliver slow, even nicotine through the skin for 16–24 hours. They’re a quiet backdrop that smooths the peaks and valleys of withdrawal. Typical starting doses range higher for people who smoke more cigarettes per day, stepping down every 2–4 weeks. Common effects include skin irritation and vivid dreams; moving the patch site and removing an overnight patch can help.
– Gum and Lozenges: Short-acting options you use when cravings strike. “Park-and-chew” (gum) or slow dissolve (lozenge) releases nicotine over 20–30 minutes. Taking one every 1–2 hours early on is common, then tapering. Mouth or throat irritation and hiccups can occur if you chew too briskly or swallow excess saliva; slower use fixes most issues.
– Inhalers and Nasal Sprays: These mimic some hand-to-mouth ritual or provide very rapid relief. They can be helpful for sudden, intense cravings, though nasal sprays may cause brief nasal or throat sting. They’re usually used alongside patches rather than alone.
Choosing a regimen depends on your smoking pattern and triggers. If mornings are brutal, a 24-hour patch may blunt that first-thing urge. If coffee breaks or commutes are your weak spots, keep gum or lozenges within reach. People who smoke within 30 minutes of waking, or smoke more than a pack daily, often do well starting with a higher-dose patch plus a short-acting product, then stepping down over 8–12 weeks. Those with sensitive skin might prefer a 16-hour patch to avoid nighttime exposure.
Practical tips raise your odds:
– Pair NRT with a quit date in the next 2–4 weeks; use products daily, not just when it feels tough.
– Schedule the short-acting doses early (e.g., every 1–2 hours) for the first couple of weeks to prevent, not chase, cravings.
– Avoid acidic drinks (coffee, soda, citrus) 15 minutes before gum or lozenge, which can reduce absorption.
– Keep a simple log of when cravings hit; match product timing to those patterns.
NRT isn’t a forever commitment. The goal is to taper as your brain recalibrates and your routines shift. If you stall or relapse, that’s information, not failure—adjust dose, timing, or product mix, and try again. Many quitters cycle through two or three attempts before it sticks; learning makes each round stronger.
Prescription Medications: Varenicline and Bupropion
Two well-studied prescription tablets—varenicline and bupropion—tackle nicotine dependence from different angles. Varenicline is a partial agonist at nicotinic receptors. It stimulates these receptors just enough to relieve withdrawal while also blocking nicotine from cigarettes, so smoking becomes less satisfying. Bupropion affects norepinephrine and dopamine pathways, reducing withdrawal and dampening cue-triggered urges. Both medications are typically started 1–2 weeks before a target quit date to reach steady levels in the body.
Effectiveness is strong in aggregate data. Multiple large trials and systematic reviews find that varenicline can raise long-term quit rates roughly two- to three-fold over placebo, especially when paired with behavioral support. Bupropion also improves outcomes, often in the range of one-and-a-half to two times versus placebo. Some studies suggest that combining varenicline with short-acting NRT yields an additional bump for heavy smokers, though others show similar results with varenicline alone; clinicians generally individualize based on tolerance and need.
Side effects are usually manageable and front-loaded. Varenicline commonly causes mild nausea or vivid dreams; taking it after food and water, and adjusting evening timing, often helps. Bupropion can bring dry mouth or insomnia; morning dosing and avoiding late caffeine may reduce sleep disruption. Bupropion is not suitable for people with a seizure disorder or certain eating disorders. For both medications, anyone with significant mood symptoms should discuss monitoring plans. Pregnant individuals and adolescents should seek tailored medical guidance for any pharmacotherapy.
Who might consider these options?
– If you’ve tried NRT without enough relief, varenicline can blunt the “reward” of cigarettes and quiet stubborn cravings.
– If you prefer a tablet and also want help with energy and concentration early in quitting, bupropion may fit.
– If mornings are toughest, or you have strong cue-driven smoking, a prescription plus short-acting NRT can cover both baseline and spikes.
– If cost is a concern, ask about generic versions and coverage; many programs reduce out-of-pocket expense.
Practical points:
– Pick a quit date 7–14 days after starting the medication; use that time to practice delaying cigarettes and trimming triggers.
– Combine with counseling; the medication quiets the biology, and coaching rewires habits.
– Plan for 12 weeks, reassess, and extend if you’re still benefiting and tolerating it well.
– If you slip, keep taking the medication; it can quickly turn a stumble into renewed traction.
Behavioral Supports, Digital Tools, and Everyday Add‑Ons
Quitting sticks better when you pair medicines with skills. Counseling—whether brief advice in a clinic, a telephone quitline, group sessions, or one-on-one coaching—roughly doubles success compared with going it alone. The mechanism is practical, not mysterious: you learn to identify your highest-risk moments, script replacements, and recover faster after slips. Four to eight touchpoints over the first two months can make a measurable difference, and many services are free or low cost.
Digital tools extend that support into your pocket. Well-designed apps and text programs nudge you during high-risk windows, track streaks, and offer quick coping exercises for cravings that hit out of nowhere. Look for features such as:
– Personalized quit-date planning with taper options if cold turkey feels daunting.
– Real-time craving logs that suggest tailored strategies rather than generic tips.
– Push reminders tied to your triggers (morning coffee, commute, after meals).
– Access to live chat or call-back coaching from trained specialists.
– Integrated cost savings and health milestones to reinforce progress.
Low-tech tools help, too. A paper tracker on the fridge can map cravings by time and mood. A small notebook can capture your “why” and a handful of fast-acting rituals to swap in—slow breathing, a quick walk, sugar-free mints, or an engaging task that occupies your hands for five minutes. Simple environmental tweaks reduce friction: keep cigarettes out of the house, clean the car to remove smoke cues, change your morning route to avoid the corner shop, and ask friends not to offer you a smoke while you’re in the early stretch.
Some people like feedback devices such as carbon monoxide (CO) breath sensors. Seeing numbers drop can be surprisingly motivating in the first week, when feelings wobble but progress is real. Others assemble a “quit kit”: water bottle, mints or gum, a stress ball, and a printed list of three quick wins to try before reaching for nicotine. The right mix is whatever makes the next urge easier to beat than lighting up.
To turn intention into action, stack habits:
– Pair morning coffee with a patch check and a two-minute breathing exercise.
– Replace smoke breaks with a timed walk and a lozenge during workdays.
– Use a “If I crave, then I will…” plan, rehearsed out loud, for your top three triggers.
– Celebrate tiny victories daily; reinforcement matters more than perfection.
The takeaway: medications lower the volume on cravings, but daily routines rewrite the soundtrack. Combine both, and your odds improve substantially—without white-knuckling every hour.
Harm Reduction, Emerging Options, and Your Next Step (Conclusion)
Not every product fits every person, and some options sit in a gray zone. E‑cigarettes deliver nicotine without smoke, and several randomized trials have shown higher quit rates compared with certain traditional NRT setups when both are paired with counseling. At the same time, long‑term respiratory and cardiovascular effects are still being studied, device quality varies, and youth uptake is a real concern. If you consider this path, treat it as a structured, time‑limited quit aid with a plan to taper nicotine—not a new hobby—and avoid dual use with cigarettes, which erodes benefits.
Nicotine pouches are smoke‑free and spit‑free; they avoid combustion but still deliver nicotine and can sustain dependence. Some people use them as a short‑term bridge away from smoking in social or high‑trigger settings, ideally alongside a taper schedule. Heated tobacco products still involve tobacco and can produce harmful emissions; they are not a risk‑free alternative, and switching without a quit plan may simply repackage the problem. “Herbal” or non‑tobacco cigarettes still produce smoke and toxins—swapping one burned plant for another is not a protective strategy.
Another medication to know about is cytisine, available in some regions. It acts on similar receptors as varenicline and has shown promising quit rates compared with placebo and, in some studies, parity or non‑inferiority to certain established therapies. Availability and guidance differ by country, so a clinician’s input is important if you have access and are curious.
Methods like acupuncture or hypnosis have devoted followers, but consistent, high‑quality evidence is limited. If you try complementary approaches, anchor them to a core plan with proven elements—NRT or prescription support plus behavioral coaching—so you’re not relying on hope alone. Safety first: if you’re pregnant, under 18, or managing complex medical or mental health conditions, personalized advice is essential before starting any nicotine or prescription product.
How to choose your path, step by step:
– Pick a quit date within the next month; tell one ally who will check in.
– Choose one “background” aid (patch or a prescription) plus one “rescue” aid (gum, lozenge, or inhaler).
– Line up support: a quitline, brief counseling, or an app with live coaching.
– Map your top three triggers and write a 60‑second action for each.
– Plan a 12‑week horizon; review progress every two weeks and adjust dose or tools.
Conclusion for you, the would‑be quitter: your goal isn’t to be a different person overnight—it’s to make the next craving easier to beat than lighting up. Products give your brain a fair fight; coaching gives your habits a new groove. Put them together, and you create momentum that survives bad days, busy weeks, and surprise triggers. Start small, start soon, and keep iterating; the road isn’t perfectly straight, but it does lead somewhere better, and you’re already facing in that direction.